Breast cancer remains one of the most common cancers affecting women worldwide. Despite growing awareness, misconceptions persist that can deter early diagnosis and effective treatment.
Experts have always advocated early detection, saying it significantly increases the chances of successful treatment.
5 common signs to watchout for:
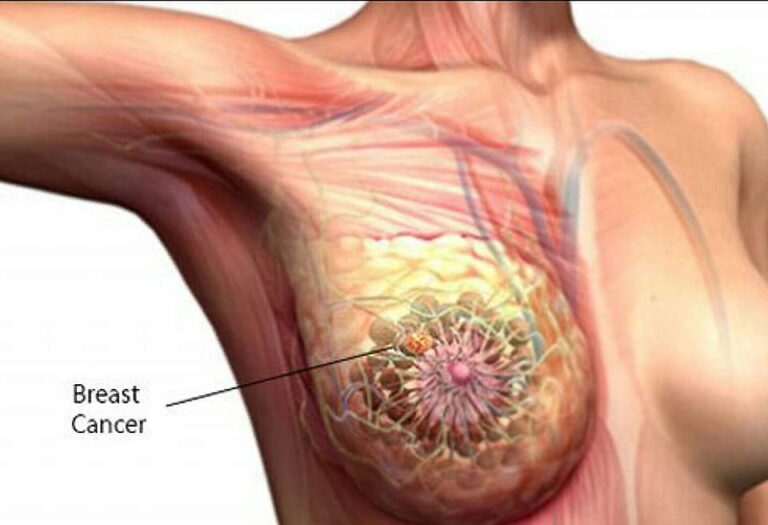
1. Lumps in the breast or underarm: A hard mass or lump that feels different from the surrounding tissue is a common early indicator. Not all lumps are cancerous, but medical evaluation is crucial.
2. Changes in breast shape or size:
Noticeable alterations in the size, shape, or contour of the breast, especially if it’s unexplained, should be checked.
3. Skin changes: Redness, dimpling (resembling the skin of an orange), or unusual skin texture on the breast may be warning signs.
4. Nipple discharge: Discharge from the nipple that isn’t related to breastfeeding, particularly if it is bloody or clear, should prompt medical advice.
5. Pain: While most breast cancers are not painful in the early stages, any persistent or unusual discomfort warrants attention.
Several myths surrounding breast cancer can hinder early detection or cause unnecessary anxiety.
Here, we separate fact from fiction:
Myth 1: Only women with a family history are at risk
Fact: While genetics play a role, most cases of breast cancer occur in women without a family history. Lifestyle factors, age, and environmental exposures also contribute to risk.
Myth 2: Wearing underwire bras increases cancer risk
Fact: There is no scientific evidence linking underwire bras to breast cancer. This myth likely originated from unfounded claims about restricted lymph flow.
Myth 3: Breast cancer always presents as a lump
Fact: While lumps are common indicators, they are not the only signs. Changes in skin, nipple position, and unexplained breast pain can be early indicators of breast cancer.
Myth 4: Men can’t get breast cancer
Fact: While rare, breast cancer can and does occur in men. The lack of awareness often leads to late diagnoses, making education crucial for all genders.
Breast cancer treatment has advanced significantly, offering better outcomes and quality of life for patients. Innovations include:
Targeted Therapy: Drugs like HER2 inhibitors target specific cancer cells, leading to more effective and less toxic treatments.
Immunotherapy: Harnessing the body’s immune system to fight cancer has shown promise, particularly in cases where conventional treatment is less effective.
Improved Surgical Techniques: Options such as lumpectomies and sentinel lymph node biopsies help preserve more of the breast and minimize invasive procedures.
Early detection remains the most critical factor for successful treatment.
Methods such as mammograms, breast MRI, and genetic screening (for high-risk individuals) are pivotal tools in catching the disease before it progresses. Health experts recommend that women conduct monthly self-exams and follow their doctor’s advice on regular screenings based on age and risk factors.
A Consultant General Surgeon, Dr. Arinzechukwu Mosanya, while speaking with The Punch, underscores the necessity of early detection.
He said, “Breast cancer is more common in older females than in young females. The older a woman gets, the higher the chances of developing breast cancer. A lifestyle that is not healthy can also predispose women to cancer.”
Addressing common misconceptions, a Consultant Radiation and Clinical Oncologist, Dr. Omolola Salako, clarifies that breast cancer is not a death sentence.
In an interview with The Guardian, she said, “Being diagnosed with breast cancer is NOT a death sentence. With the scientific and social progress in breast cancer care, more women are surviving breast cancer in Nigeria and worldwide.”
Also, a Consultant Clinical Oncologist, while discussing the evolution of breast cancer treatments with The Punch, said, “Surgical treatment traditionally was mastectomy and clearing the axillary lymph nodes but recent advances now allow breast-sparing surgeries and sentinel lymph node sampling.
“Chemotherapy has been around for a long time but still effective. However, due to improvements in genetics and molecular sampling, more targeted therapies and immunotherapy are being used which are more effective than chemotherapy with lesser side effects.”